Biceps Tendon Rupture in Climbers

Truckee, CA. 📷 Jason Hsieh
You’re at the crux. Left elbow is locked off at your side, right hand clutching a shallow intermediate. You‘ve been here before, numerous times in fact. Bumping the right hand to the above edge will surely get you the send. You release your right hand to bump—pop. Left hand releases from the wall as you free fall. You immediately grasp your left arm as pain overcomes your elbow. You inspect your arm and notice something is off. You try to bend your elbow and notice it is hard to lift. As minutes pass you notice some swelling around the elbow and the severe pain you felt minutes ago slowly subsides to a dull ache. What happened?
The scenario above describes a climbing specific mechanism of injury to the biceps tendon when a lengthening bicep muscle is subjected to excessive loads and detaches from one or more of its attachments. Although this type of injury is rare among climbing athletes, this article provides both climbers and clinicians a guideline to identify the injury if it occurs. Additionally, it provides a guideline to help understand the course of conservative rehab following surgical intervention of a distal biceps tendon rupture.
Signs and Symptoms
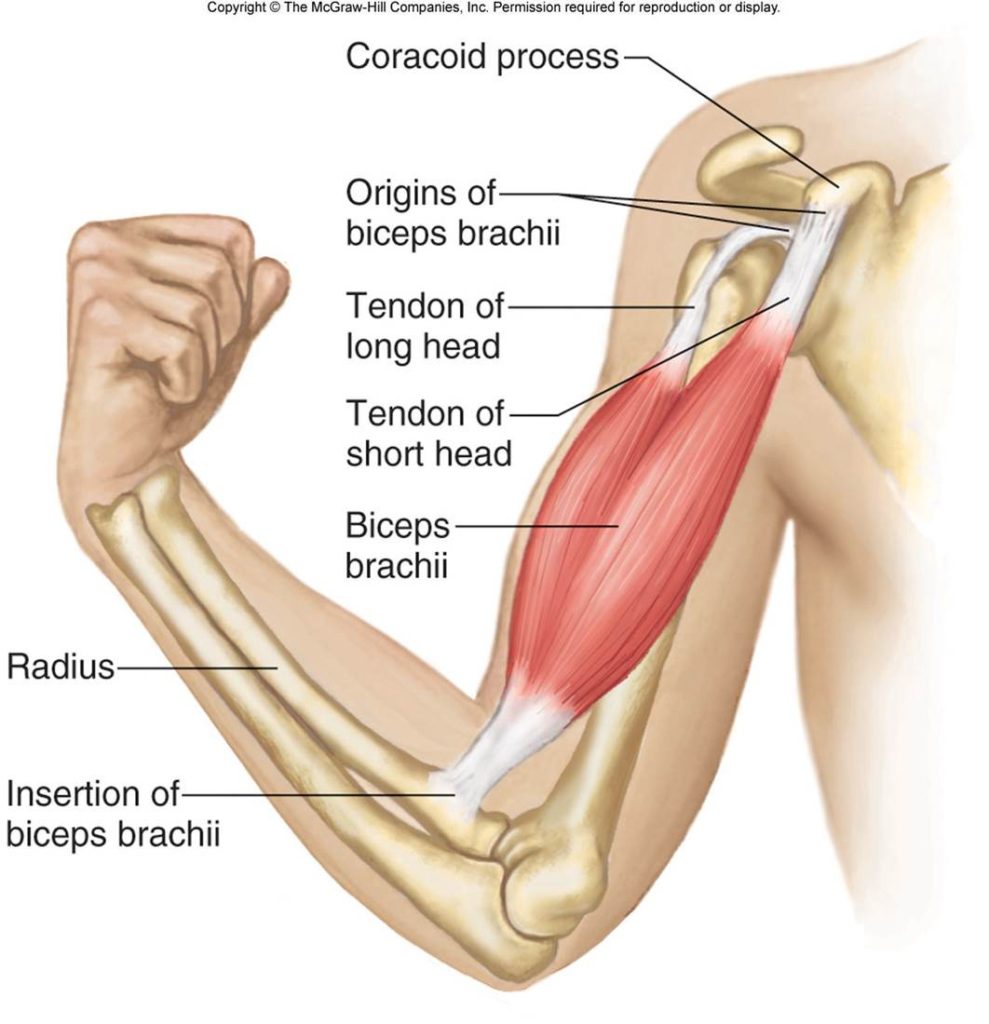
Figure 1 Anatomy of biceps brachii. McGraw-Hill Companies Inc.
To make sense of the signs and symptoms following this injury, we need to explore the muscle’s anatomy and function.
The biceps muscle (known formerly as biceps brachii) begins as two distinct muscle bellies from its origin and converges near the mid-shaft of the humerus into a single muscle where it inserts onto the forearm bone (Figure 1). The inner belly is the short head while outer belly is the long head. The short head originates from the coracoid process of the scapula, whereas the long head originates from the supraglenoid tubercle, tucked in a thick connective tissue that envelopes the rim of the shoulder joint. This comprises the “socket” portion of the “ball and socket” shoulder joint. This makes the proximal tendon of the long head of the biceps brachii unique because it is continuous with the shoulder labrum. By contrast, most tendons attach directly to bone. Once past the mid-shaft of the humerus, both muscle bellies converge inferiorly to a single muscle tendon where it inserts onto the radial tuberosity of the forearm.
The biceps brachii is a multi-joint muscle, spanning across at least two joints (shoulder and elbow) to allow various functional motions. Elbow flexion is the primary action of the biceps. Its lesser-known actions include, forearm supination, distally, and minor shoulder flexion, proximally. The biceps muscle allows us to perform daily tasks, such as bring food to your mouth (elbow flexion), tightening a screw with a screwdriver with the right hand (forearm supination), and raising your arm to give your climbing partner a fist bump (shoulder flexion).
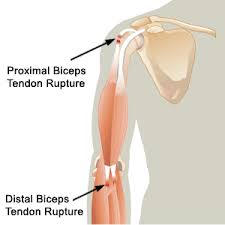
Figure 2 Most common bicep rupture sites. Source: www.5280cryo.com
Upon rupture of the biceps tendon, a distinct clinical presentation will exist. Figure 2 depicts the most common sites where the biceps tendon is likely to rupture.
These associated signs and symptoms of complete biceps tendon rupture may include:
- Pain and tenderness
- Swelling
- Marked weakness at the elbow and shoulder
- Limited elbow ROM
- Upper arm deformity
If you present with a cluster of these specific signs and symptoms, you should seek professional help from a medical practitioner. Upon examination, several tests and measures exist to confirm the diagnose of biceps tendon rupture.
Assessment
Diagnosing a biceps tendon rupture begins with a detailed subjective history of the trauma, followed by a thorough physical examination that include palpation of the affected region and performance of a cluster of special tests.
Some subjective complaints may include:
- Hearing a loud pop
- Immediate severe pain around elbow/shoulder region following trauma
- Severe pain subsiding to a dull ache after 20 minutes of rest
- Inability to bend elbow
Observation and palpation:
- Tenderness over the anterior region of the elbow (distal injury)
- Inability to flex elbow through ROM
- Upper arm deformity due to a retracted bicep muscle belly (“popeye deformity”)
Your physical therapist or other healthcare professional may perform a cluster of the following special tests when a biceps tendon rupture is suspected:
- Biceps squeeze test
- Bicipital aponeurosis flex test
- Hook test
- Passive forearm pronation test
- Biceps crease interval test
If a qualified clinician requires further confirmation, diagnostic imaging may be required such as dynamic ultrasound or magnetic resonance imaging (MRI).
Surgical intervention
Once a biceps tendon rupture has been confirmed, treatment almost always results in surgical intervention unless impairments do not severely restrict participation in functional activities, like in some cases of proximal biceps tendon ruptures.1 However, it is recommended that most individuals with a prior high level of functional activity undergo surgery to regain their desired performance.
The type of surgery depends on if the rupture occurred proximally or distally. Distal biceps rupture typically involves refixation of the tendon onto the radial tuberosity using a combination of absorbable anchors and/or sutures. This procedure is minimally invasive, low risk of complications and associated with good clinical outcomes.2 While a standard procedure for distal biceps tendon repair exists, consensus for proximal biceps tendon repair is lacking; therefore, there are several options. Widely used for its favorable biomechanical conditions is a biceps tenodesis where the long head tendon is fixated proximally on the humeral bone. Another technique, known as the bicep tendon transfer, adjoins the long head tendon with the short head tendon at the coracoid process. Caution should be taken with the latter technique as some studies have linked it to the development of subacromial impingement.3
As always, surgical candidates should discuss their long-term goals with their surgeon as well as weigh the pros and cons of all available surgical methods to maximize recovery potential and ensure return to desired functional activity.
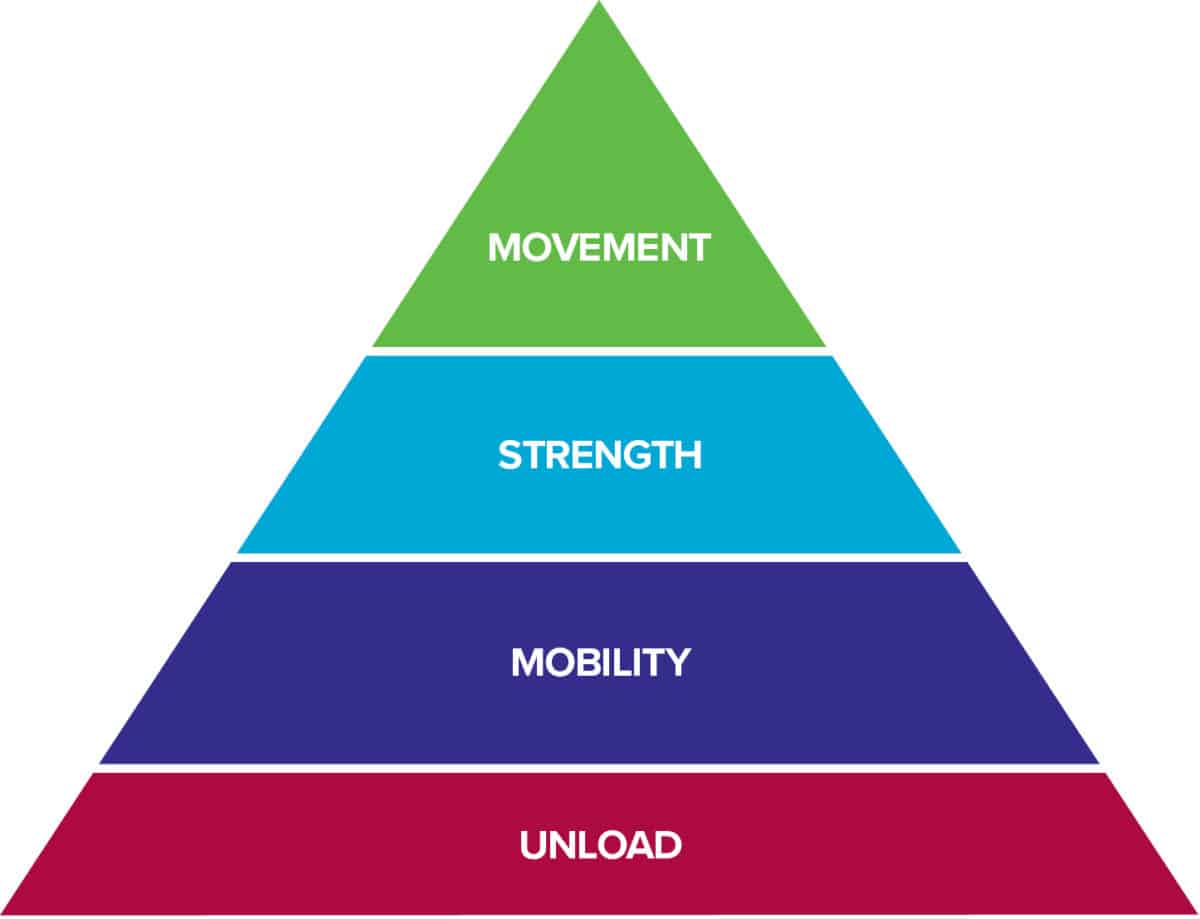
The Rock Rehab Pyramid
Following surgery, one can expect a relatively moderate length of rehabilitation requiring physical therapy anywhere from 8 to 14 weeks before engaging in low-level sport-specific activity. The rehabilitation outlined below follows and is adapted from the Brigham and Women’s Hospital distal biceps tendon repair protocol.4 The protocol closely resembles the principles of the Rock Rehab Pyramid that begins by addressing the inflamed tissue then gradually introducing mobility, strength and, in the late stage, movement. These guidelines serve as a general outline for recovery and should not replace the clinical decisions made by your surgeon or physical therapist. Progressions to, adaptations to or dosage of rehabilitation should be made based on the individual’s progress, objective physical exam findings, and/or presence of post-operative complications.
Abbreviations:
AROM: active range of motion
PROM: passive range of motion
ROM: range of motion
Consult with Your Surgeon and Doctor of Physical Therapy
This protocol is for informative purposes only. Exercises and recommendations within the protocol should only be followed with approval from your doctor of physical therapy who will collaborate with your surgeon to determine the appropriate exercises and time frames to progress.
Phase I (Post-operative days 5 – 7)
The focus of phase I is to allow enough time for the surgical site to heal. To ensure uninterrupted healing, surgeons will place the elbow in a splint to restrict its motion that would otherwise place unwanted tension on the surgical attachment site. A rigid, posterior splint, shown in Figure 3, is commonly used to place the elbow in 90 º of flexion with the forearm in neutral.

Figure 3 Posterior splint. Source: www.rehab-store.com

Figure 4 Hinged elbow ROM brace. Source: www.orthomen.com
Phase II (Weeks 2 – 3)
The focus of phase II is to begin restoring mobility and initiating PAIN-FREE, submaximal isometric exercises targeting both shoulder and elbow musculature. During this period, the elbow is placed in a hinged elbow ROM brace, shown in Figure 4. The brace set is unlocked between 45º to full flexion ROM to permit greater motion, but not to exceed excessive elbow extension passed 45º.
- Week 2:
- Passive elbow flexion within 45 º to full flexion; passive supination with elbow at 90
- To be performed by a physical therapist
- Passive elbow flexion within 45 º to full flexion; passive supination with elbow at 90
-
- [Video below] Assisted ROM for elbow extension
- Frequency: daily
- Intensity: holding 1 lb. dumbbell for 5 reps
- Time: 20 – 30s hold per rep
- [Video below] Assisted ROM for elbow extension
- [Video below] Shoulder 6-way isometric (ER, IR, FLX, EXT, ABD, and ADD) with elbow at 90 º of flexion
- Frequency: Daily
- Intensity: Perform sub-maximally for 3 sets of 8 – 12 reps
- Time: Hold for 20 – 30s per rep and cycle through all directions before beginning next set
- [Video below] 3-way bicep isometrics with forearm in supination, neutral and pronation
- Frequency: Daily
- Intensity: Perform sub-maximally for 3 sets of 8 – 12 reps
- Time: Hold for 20 – 30s per rep and cycle through all directions before beginning next set
- Week 3
- Initiate active-assisted ROM elbow flexion
- Continue assisted extension and progress to extension PROM
- [Video below] Single plane AROM elbow flexion, extension, supination and pronation
- Frequency: Daily
- Intensity: Perform sub-maximally for 3 sets of 8 – 12 reps
- Time: Rest 30 seconds between sets
Phase III (Weeks 4 – 14)
The focus of phase III is re-introducing combined motions and strengthening the biceps muscle. At this phase, the climber may begin low-grade climbing.
- Week 4 – 8:
- Hinged elbow brace progression:
- Week 4: 30 to full elbow flexion
- Week 5: 20 to full elbow flexion
- Week 6: 10 to full elbow flexion
- Week 8: full ROM of elbow; discontinue brace if rehab milestones are met
- Continue with single plane AROM exercises
- May begin combined/composite motions
- More aggressive ROM management may be required if ROM deficits persists; consult referring surgeon
- Hinged elbow brace progression:
- Week 8 – 10:
- Increase intensity of ROM and strength exercises while decreasing frequency to allow adequate rest
- [Video below] Initiate resisted elbow flexion, extension, supination and pronation
- Frequency: 3 – 4x/week
- Intensity: Using resistive bands perform 3 sets of 8 – 12 reps
- Time: Rest 30 – 60 seconds between sets
- [Video below] Initiate isometric bar pulls with forearm in full supination, neutral, and pronation with counterweight using digital/analog bodyweight scale
- Frequency: 3 – 4x/week
- Intensity: Unweight 30-50% of bodyweight for 10 reps
- Time: Hold for 20 – 30 seconds per rep and rest 60 seconds between sets
-
- Begin easy slab or vertical climbing avoiding overhanging walls and undercling holds; limit sessions before onset of muscular fatigue
- Week 10:
- Begin supervised hangboard training with elbow in full extension to condition fingers for return to climbing activity (consult a trainer or physical therapist familiar with climbing training to implement the use of a pulley to offset body weight)
- Weeks 12 – 14
- Initiate light upper extremity weight training
- Begin moderate vertical climbing and easy overhung climbing with good footholds; limit sessions before onset of muscular fatigue
If you’re suspecting a biceps tendon rupture, seek immediate medical help. Once properly diagnosed and surgical intervention is decided, rehabilitation should begin as soon as possible under the guidance of a doctor of physical therapy in collaboration with your surgeon. This article provides a rough guideline that begins with a period of immobilization (unloading) following surgery. This is then followed by a period of regaining range of motion (mobility) combined with submaximal isometric strengthening. In the late stages, strengthening is progressed and climbing specific activities re-introduced. Although not guaranteed, climbers should be able to regain their initial level of climbing within the first year.5
The Research
- Klonz A, Loitz D, Wöhler P, Reilmann H. Rupture of the distal biceps brachii tendon: Isokinetic power analysis and complications after anatomic reinsertion compared with fixation to the brachialis muscle. J Shoulder Elb Surg. 2003;12(6):607-611. doi:10.1016/S1058-2746(03)00212-X
- Loitz D, Klonz A, Reilmann H. Technik der gedeckten refixierung der distalen bizepssehne. Unfallchirurg. 2002;105(9):837-842. doi:10.1007/s00113-002-0432-5
- Ambacher T, Winter E, Mayer F. Muscle strength after surgical treatment of ruptures of thfile:///C:/Users/zesul/Desktop/Climbing SIG/Blog Entry/Biceps_Tendon_Ruptures_in_Rock_Climbers.10.pdfe long biceps tendon by refixation to the short head. Sport Sport. 1999;13:90-95. doi:10.1055/s-2007-993322
- Wilcox III RB. Biceps Tenodesis Protocol Biceps Tenodesis Protocol. 2009;21(11):1-5.
- Schöffl VR, Harrer J, Küpper T. Biceps tendon ruptures in rock climbers. Clin J Sport Med. 2006;16(5):426-427. doi:10.1097/01.jsm.0000244607.54017.55
About the Author
Zeno Lee is a physical therapist working and residing in San Joaquin Valley of California. He was pulled into the world of rock climbing by his grad school peers in 2018. His Olympic lifting background naturally drew him into indoor bouldering. More recently, he has discovered a deeper appreciation for outdoor sport climbing. When not climbing, he enjoys spending time with friends and family, cooking, and training his four-legged companion, Zoey.
If you have questions, feel free to email Zeno at zesulee@gmail.com.
- Disclaimer – The content here is designed for information & education purposes only and the content is not intended for medical advice.


Nice job, Zeno!
Hi Zeno,
I’m about to go for this op after rupturing my bicep last week, really solid article, and gave me loads of insight and hope for a strong comeback. Nice one. Phill