The Gym Boulder’s Guide to Preventing Lower Body Injuries While Jumping/Landing/Falling
Are you sending hard only to jump off and twist your ankle and/or knee? Day 1 in the boulder gym we all learn proper falling technique, “gently land with your knees bent and roll to your butt…” but… how many of us actually do that on a regular basis..? Unless you down-climb 100% of the time, most of us are jumping and/or falling 20+ times per gym or outdoor session at distances anywhere from 1-10ft, sometimes greater. Because we don’t live in a perfect world where we all land perfectly every time the following are several strategies and cross training progressions to prevent lower extremity (foot/ankle, knee, and hip) injuries while landing.
Lower Body Injury Risk Factors
Bouldering poses obvious injury risks, especially for the lower body, identifying potential risk factors is often the easiest way to prevent future injury.1,2 Landing safely from a variety of heights planned and/or unplanned requires quick thinking, balance, and coordination. When considering risk factors we must consider environmental factors and individual factors.3
Environmental factors that increase risk of injury during falling/landing include:
- Mats
- Climbing shoes
- The climb itself
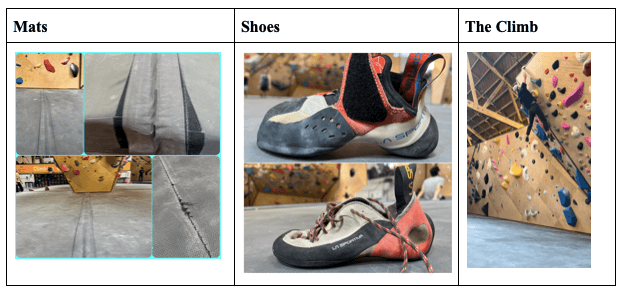
Not only do gym mats require increased time to stabilize the lower extremities upon landing; gym mats come in a variety of different densities, thicknesses, ages, degrees of damage/repairs, and seams which all pose added risks. Additionally, climbing shoes, and the severity of downturn in one’s shoe poses the added risk of landing on the side of the foot and turning the ankle. Furthermore, slick footholds and unexpected falls due to the nature of the holds and setting during a climb increase risk of injury during fall/landing.
Individual factors that increase risk of lower body injury during falling/landing include:
prior history of injury that increases lower extremity instability or genetic hypermobility/instability.4,5
poor coordination or poor neuromuscular control of dynamic stabilization of the lower extremity.4,5
personal choice of landing on feet rather than the shock absorption roll mentioned earlier.
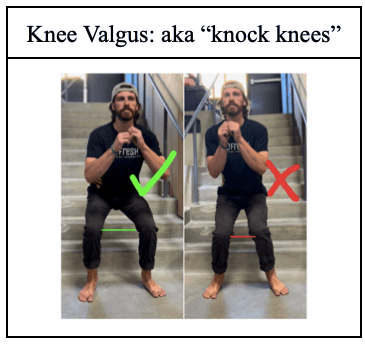
Prior history of foot/ankle, knee, and or hip injury, in general, causes instability of the joint and decreases proprioceptive control during balance activities. Genetic hypermobility/instability of lower extremity may also be present in those with connective tissue dysfunction; such as those with Ehlers Danlos Syndrome or Marfan Syndrome. Poor coordination/neuromuscular control of lower extremities during dynamic stabilization includes increases in knee valgus or “knocked knees” during landing. Lastly, individual factors include personal choice to stick a landing on one’s feet, choice of height at which one is jumping from, and choosing to turn or twist during jump. 70% of ACL injuries are non-contact injuries, meaning they are caused by movement patterns of the individual.6 ACL injuries often occur when the foot is firmly planted and undergoes a sudden change of direction.7 Turning while jumping down inherently increases risk for ACL injury.
Assessment
In order to decrease risk of injury during falling and landing when bouldering one must assess one’s risk factors both environmental and individual. Environmental factors are quick and easy to assess each climbing session.3 Individual factors are slightly more challenging to assess, and for formal assessment/medical diagnoses it is recommended to see a healthcare provider.
Environmental Factors to Assess
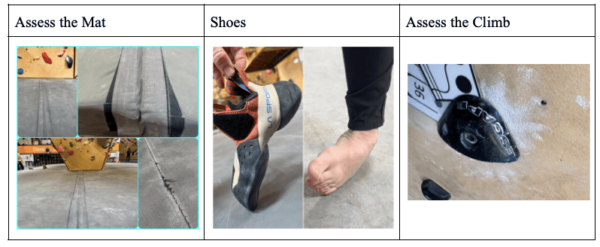
- Assess the mat – Get familiar with the mat: density, thickness, damages, repairs, seams, and mat placement when outdoors.
- Shoes – Notice if your shoes have a severe downturn – putting your ankle in a more turned in position
- Assess the Climb – Look for slick holds, look for the crux/potential falling points, and direction you may fall or land in.
Individual Factors to Assess
1. Prior History of Injury
- Ankle instability: Talar Tilt Following a common ankle sprain, ie. twisting/rolling your ankle the ligaments along the outside of the ankle get over stretched, a quick easy way to assess is by performing a talar tilt test. It is best to compare to the uninvolved side in order to determine if there is increased laxity following an ankle sprain. For confirmation please see an orthopeadic healthcare professional.
- Knee Instability: In order to assess instability in the knee it is highly recommended you are assessed by an orthopeadic healthcare professional.
2. Genetic Hyper Mobility/Instability/Dislocation/Subluxation
- Genetic Hypermobility/Instability is more common than you might think, it may include such diagnoses as Eler’s Danlos Syndrome or Marfan’s Syndrome. However, many people are just genetically predisposed to have increased laxity throughout their joints. Easiest way to identify general hypermobility, look for hyperextension in multiple joints; such as the knee, elbow, and thumb.
- Chronic Dislocations/Subluxations – In more severe cases people with genetic hypermobility disorders will experience chronic dislocations and or subluxations, where the joint “pops out and quickly pops back in.” If this is something you’ve experienced, or is a concern for you, it is recommended to see a healthcare professional for formal diagnosis.

3. Neuromuscular Control (coordination of balance)
- Rhomberg Test: is a quick easy test to examine one’s static balance – otherwise known as balance when not moving. While falling and landing during climbing is a dynamic movement, it is often recommended to achieve proficiency in static balance prior to dynamic balance first with eyes open followed by eyes closed. It is recommended one is able to maintain balance in the different scenarios for 30 seconds.
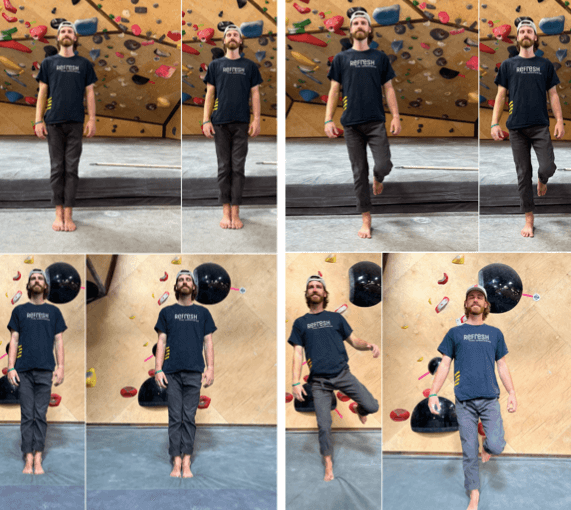
- Dynamic Balance with Landing Error Scoring System (LESS): The LESS is a specific test to determine risk of injury based on the individual’s movement pattern while landing a jump.8 The official version of the LESS is quite extensive and requires a specific camera set up. For our purposes we recommend recreating something similar with your phone camera in front of the person performing a drop landing. See video for example. Film yourself performing drop landing on both a flat/firm surface and mat/squishy surface
4. Choice of Jump
- Sticking landing on feet vs rolling: It is highly recommended, best way to avoid any injury – bend the knees absorb shock and roll
- Height of Jump: If possible, it is recommended to down-climb as much as you can either fully to the ground or to reduce the height of the jump
- Turning While Landing: Planting the foot while turning/rotating severely increases your risk of knee injury specifically ACL injury.
Progressing Lower Body Stabilization
Progression of lower body stabilization needed in bouldering can be a slightly tedious undertaking, below this process is broken down into three stages.4,5 The stages can be performed in a variety of patterns and orders, which depends on one’s current level of training and/or whether someone is returning following lower body injury. In order to improve balance and coordination in your landing it is recommended to perform exercises 2-4 days per week. Check out the videos for more information.
Recommendation for uninjured climber looking to prevent future injury
- Focus on increasing lower body strength and awareness. Workouts should be challenging yet doable, thus there may be some mix and match of the progression. It is recommended to begin with Stage 1, however once you’ve gained proficiency, it may also be used as a warm up to either landing training, lower body training, and/or prior to bouldering session. Stages 2 and 3 may be performed simultaneously, find a level of Stage 2 and 3 that is most challenging, and work at that until you are proficient.
Recommendation for injured climber returning to bouldering
- When returning to sport following injury it is important to maintain a pain free experience with your workouts. Pain free includes mid-workout as well as no increases in pain later that day or the next day. Normal muscle soreness is okay, however increases in your symptoms you may be performing exercises incorrectly and/or too high of volume and/or too high resistance.
- GO EASY! Begin with Stage 1, it is recommended that you are proficient and feel strong at Stage 1 prior to progressing to Stage 2. You may however, perform all exercises in Stage 1 simultaneously. Stages 2 and 3 however, it is recommended that you become proficient in each step of the stage prior to progression.
Lower Body Stabilization Progression for Bouldering
Stage 1: Basic Strength
- Squats: 3sets, 20-30reps
- Side Steps with Theraband: 3sets, 10reps
- Single Leg Heel Raises: 3sets, 20-30reps
- Single Leg Step Down: 3sets, 10-20reps
- *May be used as a warm up
- *Attempt exercises on climbing mat for added balance training.
Stage 2: Static Single Leg Balance
Practice balance on one leg
- Firm Surface
- Soft Surface
- Firm Surface Eyes Closed
- Soft Surface Eyes Closed
- *Perform 3sets, 30-60s – at a level of progression that is challenging yet doable
- * For your safety, stand near something or someone to grab on to!
- *You may use even 1 finger to provide some assistance
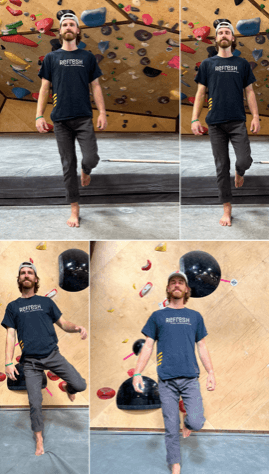
Stage 3: Dynamic Drop Landing Progression
Drop Forward → Lateral → Rotational
- Low height, firm surface, two feet
- Low height, firm surface, single foot
- Low height, soft surface, two feet
- Low height, soft surface, single foot
- High height, soft surface, two feet
- ***Heights should range from 16-42in. Higher heights should ONLY be performed using soft surface AND TWO feet landing. Landing from height above 42in NOT recommended, perform at your own risk.
- *** Landing from heights higher than 42in one should be practicing proper land and roll.
- * Have a friend film you, focus on decreasing knee collapse.
See a Doctor of Physical Therapy
For further information on rehabbing and preventing lower body injuries related to landing seek out help from a doctor of physical therapy. In many states you can see a physical therapist through direct access; meaning you may see them directly without a prescription from a medical doctor. A physical therapist may target your weaknesses and help you achieve optimal performance and prevent future injuries.
The Research
- Josephsen, G., Shinneman, S., Tamayo-Sarver, J., et al. (2007). Injuries in bouldering: A prospective study. Wilderness & Environmental Medicine, 18(4), 271–280. https://doi.org/10.1580/06-weme-or-071r1.1
- Lum, Z. C., & Park, L. (2019). Rock climbing injuries and time to return to sport in the recreational climber. Journal of Orthopaedics, 16(4), 361–363. https://doi.org/10.1016/j.jor.2019.04.001
- Shumway-Cook, A., Woollacott, M. H., Rachwani, J., & Santamaria, V. (2023). Motor control: Translating research into clinical practice. Wolters Kluwer.
- Aerts, I., Cumps, E., Verhagen, E., Mathieu, N., Van Schuerbeeck, S., & Meeusen, R. (2013). A 3-month jump-landing training program: A feasibility study using the RE-AIM framework. Journal of Athletic Training, 48(3), 296–305. https://doi.org/10.4085/1062-6050-48.3.18
- DiStefano, L. J., Marshall, S. W., Padua, D. A., et al. (2016). The effects of an injury prevention program on landing biomechanics over time. The American Journal of Sports Medicine, 44(3), 767–776. https://doi.org/10.1177/0363546515621270
- Griffin, L. Y., Hewett, T. E., & Shultz, S. J. (2007). Understanding and preventing noncontact Acl injuries. Human Kinetics.
- Wetters, N., Weber, A. E., Wuerz, T. H., Schub, D. L., & Mandelbaum, B. R. (2016). Mechanism of injury and risk factors for Anterior Cruciate Ligament Injury. Operative Techniques in Sports Medicine, 24(1), 2–6. https://doi.org/10.1053/j.otsm.2015.09.001
- Hanzlíková, I., & Hébert-Losier, K. (2020). Is the landing error scoring system reliable and valid? A systematic review. Sports Health: A Multidisciplinary Approach, 12(2), 181–188. https://doi.org/10.1177/1941738119886593
Author Information
AJ White-Graff, PT, DPT, CSCS (they/them) has a lifelong passion for anatomy, injury prevention, rehabilitation, and movement. They completed their doctorate in physical therapy at California State University Long Beach. As a 500 hour Experienced-Registered Yoga Teacher and a Certified Strength and Conditioning Specialist (CSCS) AJ has taught yoga and fitness classes throughout New York City and Los Angeles since 2010.
Currently, AJ is a full time PT at Select Physical Therapy in Long Beach, California. AJ also teaches yoga, functional alignment, strength/conditioning and injury rehab and prevention strategies to rock climbers throughout Southern California. AJ is also a proud member of the LGBTQIA+ community, and aims to create a climbing community and rehab environment that achieves inclusivity and accessibility for all individuals.

- Disclaimer – The content here is designed for information & education purposes only and the content is not intended for medical advice.