Trigger Finger Climbing
Question:
Dr. Vagy,
I am a Doctor of Physical therapy student and I wanted to ask you a climbing specific injury question. A couple of weeks ago, I woke up and my middle fingers felt a little stiff (my left hand especially). I could still make a fist, but I noticed that when I specifically flexed my middle finger individually, there was definitely a point of stiffness, and if I continued to flex past that point my finger snapped into flexion. I had no problem extending my fingers from a fist position, and that movement was smooth. I’ve been resting the fingers by taking a break from climbing, and my right hand middle finger is a somewhat better but my left hand middle finger is about the same. The stranger thing is that besides the initial period in the morning, my fingers seems to go back to normal and I have no problem doing my daily routine. There are no activities that cause pain, and palpating around my fingers doesn’t produce any pain. Even in the morning, I wouldn’t say the stiffness is super painful… it just feels, well, stiff.
Any thoughts as to what is going on? Have you seen this happen to climbers in the past? Being a younger individual, i’m trying hard to prevent any major pulley injuries. I’m really itching to go back to climbing, but I’m pretty apprehensive of potentially causing a more severe injury to myself. Let me know what you think!
Thanks,
Charles
Answer:
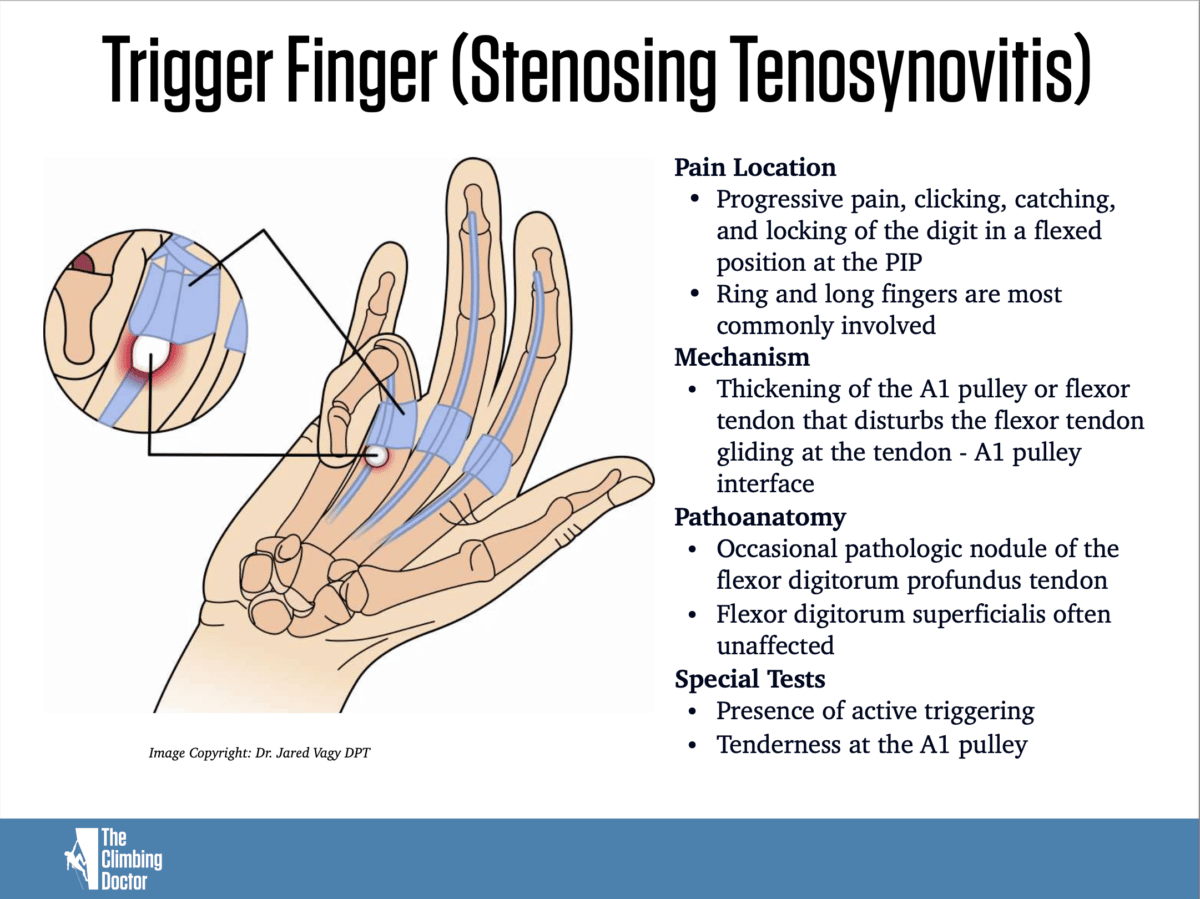
What you are experiencing doesn’t sound like a pulley injury but more like trigger finger. A pulley injury is usually mostly felt during active contraction as the flexor tendons exert an outward pressure on it. Trigger finger, is when one if your digits gets stuck in flexion and then usually extends with a snap. It is also commonly associated with morning stiffness, activities that require repetitive use of the finger flexors and most commonly affects your middle finger and thumb.
Have one of your Physical Therapy classmates take a look. If it is trigger finger, there may be a nodule that you can palpate. Try to determine the structural cause of your stiffness. Are your symptoms from tenosynovitis or may they be related to a soft tissue or joint restriction. Assess your passive range of motion and compare to the integrity of the joint mobility of each of your IP joints and MCP joint to help determine.
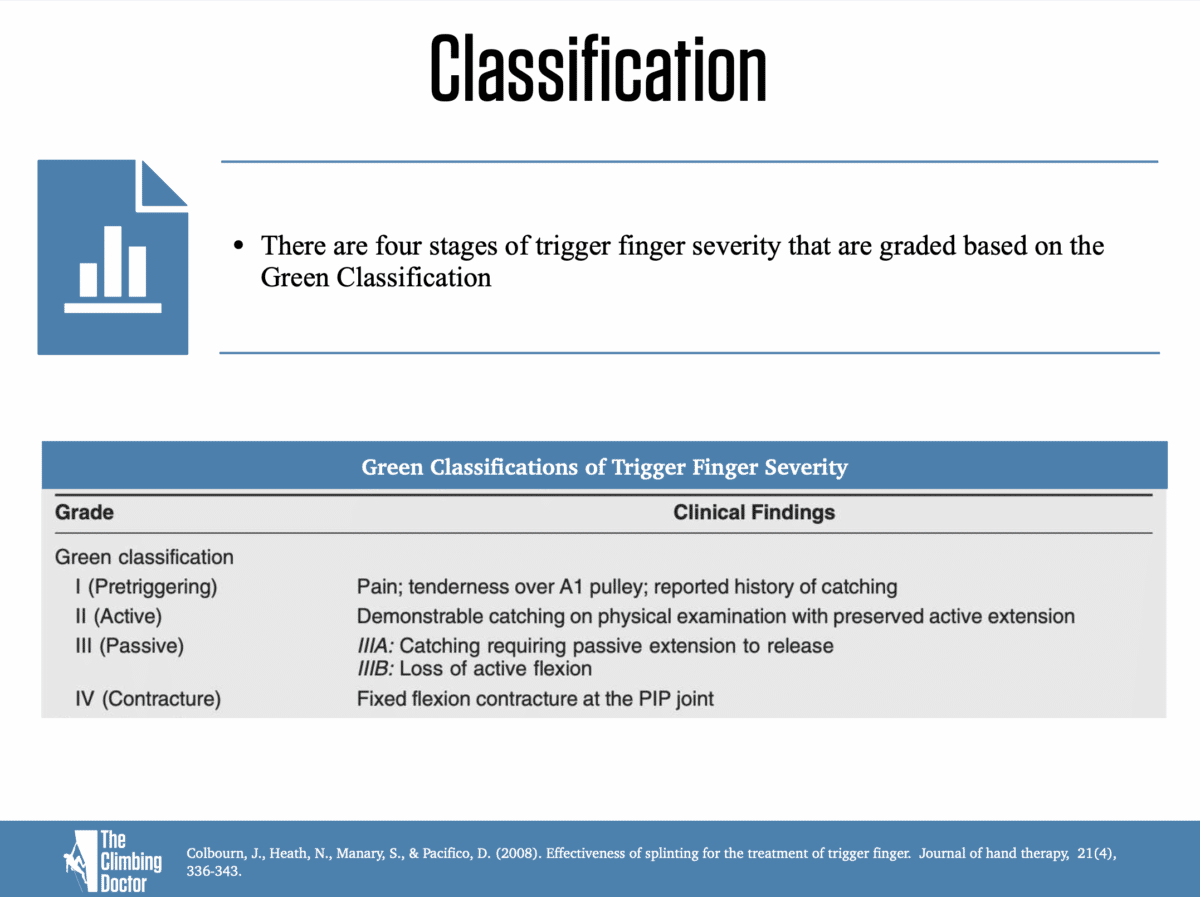
I have included two images below that explain more about the condition and classifications of trigger finger.
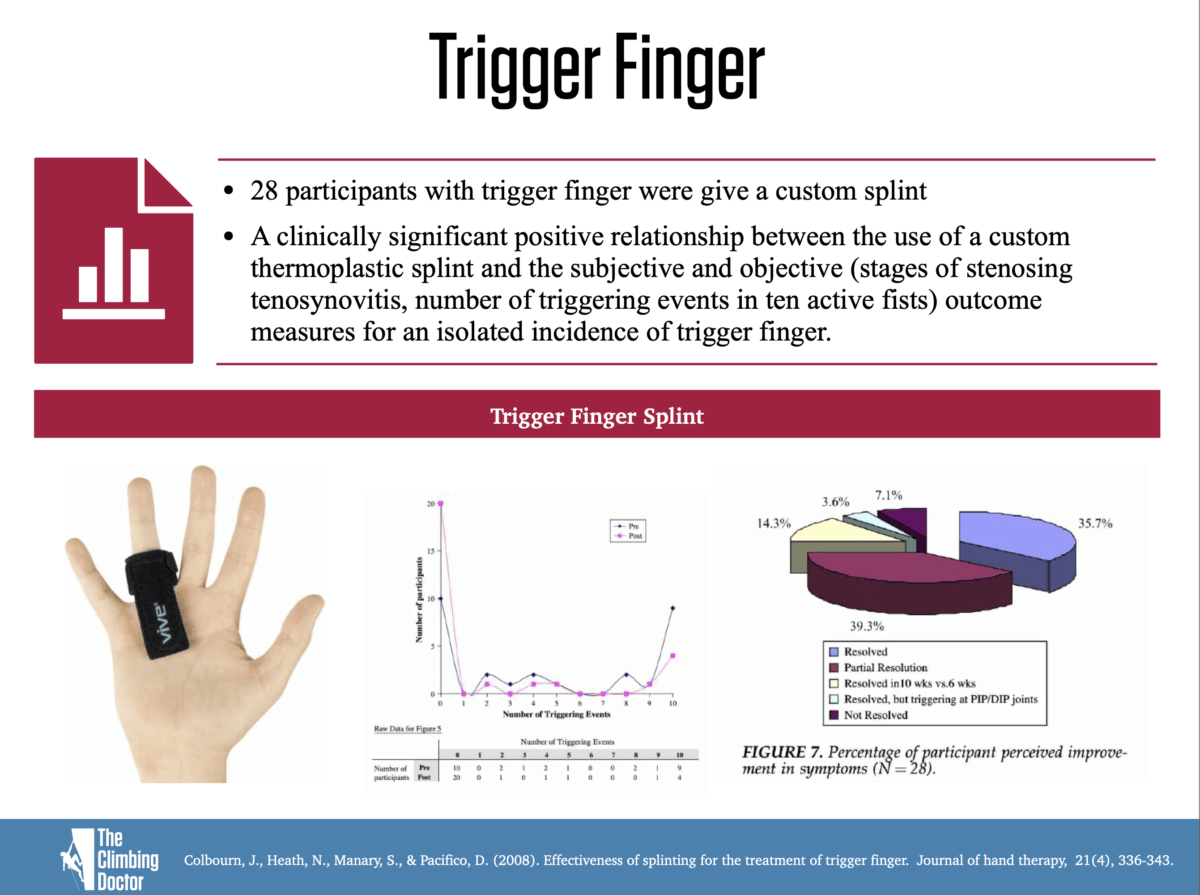
Additional, if you have diagnosed the injury as trigger finger, there has been good research to show that splinting the finger can provide improved results. In the study below:
Colbourn, J., Heath, N., Manary, S., & Pacifico, D. (2008). Effectiveness of splinting for the treatment of trigger finger. Journal of hand therapy, 21(4), 336-343.
28 participants with trigger finger were give a custom splint. A clinically significant positive relationship between the use of a custom thermoplastic splint and the patient feeling better (subjective reports) and getting better (objective findings) were documented. They improved within the stages of stenosing tenosynovitis the number of triggering events in ten active fists and isolated incidences of trigger finger.
In another study below:
Gil, J. A., Hresko, A. M., & Weiss, A. P. C. (2020). Current Concepts in the Management of Trigger Finger in Adults. JAAOS-Journal of the American Academy of Orthopaedic Surgeons, 28(15), e642-e650.
They identified best practices in the management of trigger finger.
- Immobilization of trigger finger can effectively relieve pain and improve function.
- Patients with acute onset (<3 months) of trigger finger can be prescribed a nighttime PIP or MCP joint blocking orthosis for up to 6 to 8 weeks.
- If splinting fails to resolve the symptoms, at least one corticosteroid injection (an up to 3) should be offered to all patients as long as the patient can tolerate the steroid or the injection procedure.
- If the patient fails splinting and injections, surgical release should can offered
There are more specific treatments than outlined in those articles that an occupational or physical therapist can provide, but just thought I would share some of the research on this. Additional slides are below.
Climb on,
Dr. Jared Vagy
“The Climbing Doctor”
- Disclaimer – The content here is designed for information & education purposes only and the content is not intended for medical advice.



I do have the same symptoms, could determine what are happening to tour fingers? Exactly the same what you said happens to me every morning. I am starting to get worried.
I would recommend seeing a medical provider to have it diagnosed. However, based on your comment, I decided to add more context to my answer from the original post. So I added some slides and research to help with the “what to do” if trigger finger is diagnosed. Hope that helps!
So what should I do to treat if I’m dealing with this? Should I stop climbing?
I have added some details to the post to help answer this. I’ve worked with plenty of climbers who have returned to climbing with trigger finger, but they just need to manage it while not climbing and hope it doesn’t happen when they are run-out above gear or high balling boulders.